Requirements to Donate a Kidney to a Family Member
| Kidney Transplantation | |
|---|---|
 | |
| Other names | Renal transplantation |
| Specialty | nephrology, transplantology |
| ICD-10-PCS | OTY |
| ICD-9-CM | 55.half-dozen |
| MeSH | D016030 |
| OPS-301 code | five-555 |
| MedlinePlus | 003005 |
Kidney transplant or renal transplant is the organ transplant of a kidney into a patient with end-stage kidney disease (ESRD). Kidney transplant is typically classified as deceased-donor (formerly known equally cadaveric) or living-donor transplantation depending on the source of the donor organ. Living-donor kidney transplants are further characterized as genetically related (living-related) or not-related (living-unrelated) transplants, depending on whether a biological relationship exists between the donor and recipient.
Before receiving a kidney transplant, a person with ESRD must undergo a thorough medical evaluation to make sure that they are salubrious enough to undergo transplant surgery. If they are accounted a good candidate, they can exist placed on a waiting list to receive a kidney from a deceased donor.[i] One time they are placed on the waiting list, they can receive a new kidney very quickly, or they may have to wait many years; in the United States, the average waiting time is three to five years.[2] During transplant surgery, the new kidney is commonly placed in the lower abdomen (belly); the person's ii native kidneys are not normally taken out unless there is a medical reason to practise so.[1]
People with ESRD who receive a kidney transplant mostly alive longer than people with ESRD who are on dialysis and may have a meliorate quality of life.[one] Withal, kidney transplant recipients must remain on immunosuppressants (medications to suppress the immune system) for the rest of their life to preclude their body from rejecting the new kidney.[one] This long-term immunosuppression puts them at higher risk for infections and cancer.[3] Kidney transplant rejection can exist classified equally cellular rejection or antibody-mediated rejection. Antibody-mediated rejection can be classified as hyperacute, acute, or chronic, depending on how long afterward the transplant it occurs. If rejection is suspected, a kidney biopsy should be obtained.[3] It is important to regularly monitor the new kidney's function past measuring serum creatinine and other labs; this should be done at least every three months for the rest of the person's life.[3]
In 2018, an estimated 95,479 kidney transplants were performed worldwide, 36% of which came from living donors.[4] The outset successful kidney transplant was performed by Joseph Murray in 1954; Murray was awarded the Nobel Prize in Physiology or Medicine in 1990 for his work in organ transplantation.[5]
History [edit]
One of the earliest mentions about the possibility of a kidney transplant was by American medical researcher Simon Flexner, who alleged in a reading of his newspaper on "Tendencies in Pathology" in the University of Chicago in 1907 that it would be possible in the and so-futurity for diseased human organs substitution for healthy ones past surgery, including arteries, tummy, kidneys and heart.[six]
In 1933 surgeon Yuriy Vorony from Kherson in Ukraine attempted the starting time human kidney transplant, using a kidney removed 6 hours earlier from a deceased donor to exist reimplanted into the thigh. He measured kidney function using a connectedness betwixt the kidney and the peel. His first patient died two days after, as the graft was incompatible with the recipient'south blood group and was rejected.[vii]
It was not until 17 June 1950, when a successful transplant was performed on Ruth Tucker, a 44-year-old adult female with polycystic kidney disease, by Dr. Richard Lawler[8] at Petty Company of Mary Hospital in Evergreen Park, Illinois. Although the donated kidney was rejected ten months later considering no immunosuppressive therapy was available at the fourth dimension—the development of effective antirejection drugs was years away—the intervening time gave Tucker's remaining kidney fourth dimension to recover and she lived another five years.[9]

Dr. John P. Merrill (left) explains the workings of a then-new auto called an bogus kidney to Richard Herrick (middle) and his blood brother Ronald (correct). The Herrick twin brothers were the subjects of the world's commencement successful kidney transplant, Ronald being the donor.
A kidney transplant between living patients was undertaken in 1952 at the Necker hospital in Paris by Jean Hamburger, although the kidney failed afterward three weeks.[10] The outset truly successful transplant of this kind occurred in 1954 in Boston. The Boston transplantation, performed on 23 Dec 1954 at Brigham Hospital, was performed by Joseph Murray, J. Hartwell Harrison, John P. Merrill and others. The procedure was done between identical twins Ronald and Richard Herrick which reduced problems of an immune reaction. For this and later work, Murray received the Nobel Prize for Medicine in 1990. The recipient, Richard Herrick, died eight years afterward the transplantation.[xi]
In 1955, Charles Rob, William James "Jim" Dempster (St Marys and Hammersmith, London) carried out the showtime deceased donor transplant in United Kingdom, which was unsuccessful.[ commendation needed ] In July 1959, "Fred" Peter Raper (Leeds) performed the first successful (viii months) deceased donor transplant in the UK. A yr after, in 1960, the first successful living kidney transplant in the UK occurred, when Michael Woodruff performed one between identical twins in Edinburgh.[12]
In November 1994, the Sultan Qaboos University Hospital, in Oman, performed successfully the world's youngest cadaveric kidney transplant. The piece of work took place from a newborn of 33 weeks to a 17-calendar month-quondam recipient who survived for 22 years (thank you to the couple of organs transplanted into him).[13]
Until the routine use of medication to prevent and treat acute rejection, introduced in 1964, deceased donor transplantation was non performed. The kidney was the easiest organ to transplant: tissue typing was simple; the organ was relatively like shooting fish in a barrel to remove and implant; live donors could be used without difficulty; and in the event of failure, kidney dialysis was bachelor from the 1940s.
The major barrier to organ transplantation between genetically non-identical patients lay in the recipient's immune system, which would treat a transplanted kidney as a 'non-cocky' and immediately or chronically reject it. Thus, having medication to suppress the immune organization was essential. Nevertheless, suppressing an private's immune system places that individual at greater risk of infection and cancer (particularly skin cancer and lymphoma), in addition to the side effects of the medications.
The ground for nearly immunosuppressive regimens is prednisolone, a corticosteroid. Prednisolone suppresses the immune system, but its long-term apply at high doses causes a multitude of side furnishings, including glucose intolerance and diabetes, weight gain, osteoporosis, musculus weakness, hypercholesterolemia, and cataract formation. Prednisolone alone is usually inadequate to preclude rejection of a transplanted kidney. Thus, other, non-steroid immunosuppressive agents are needed, which also allow lower doses of prednisolone. These include: azathioprine and mycophenolate, and ciclosporin and tacrolimus.
Indications [edit]
The indication for kidney transplantation is end-stage renal disease (ESRD), regardless of the primary crusade. This is defined as a glomerular filtration rate below xv ml/min/1.73 chiliad2. Common diseases leading to ESRD include renovascular affliction, infection, diabetes mellitus, and autoimmune conditions such equally chronic glomerulonephritis and lupus; genetic causes include polycystic kidney affliction, and a number of inborn errors of metabolism. The commonest 'cause' is idiopathic (i.e. unknown).
Diabetes is the most common known cause of kidney transplantation, accounting for approximately 25% of those in the Usa. The majority of renal transplant recipients are on dialysis (peritoneal dialysis or hemodialysis) at the time of transplantation. Nonetheless, individuals with chronic kidney disease who have a living donor bachelor may undergo pre-emptive transplantation before dialysis is needed. If a patient is put on the waiting list for a deceased donor transplant early enough, this may also occur pre-dialysis.
Contraindications and requirements [edit]
Contraindications include both cardiac and pulmonary insufficiency, besides as hepatic illness and some cancers. Concurrent tobacco use and morbid obesity are also among the indicators putting a patient at a higher take a chance for surgical complications.
Kidney transplant requirements vary from program to programme and country to land. Many programs identify limits on age (e.1000. the person must be under a certain historic period to enter the waiting list) and require that one must be in adept health (aside from kidney disease). Significant cardiovascular illness, incurable concluding infectious diseases and cancer are often transplant exclusion criteria. In addition, candidates are typically screened to determine if they will exist compliant with their medications, which is essential for survival of the transplant. People with mental illness and/or significant ongoing substance abuse issues may be excluded.
HIV was at i point considered to be a consummate contraindication to transplantation. There was fear that immunosuppressing someone with a depleted immune arrangement would result in the progression of the disease. Withal, some research seem to suggest that immunosuppressive drugs and antiretrovirals may work synergistically to help both HIV viral loads/CD4 prison cell counts and prevent active rejection.
Sources of kidneys [edit]
Since medication to prevent rejection is so effective, donors do not need to be similar to their recipients. Most donated kidneys come from deceased donors; still, the utilisation of living donors in the United States is on the rise. In 2006, 47% of donated kidneys were from living donors.[14] This varies by country: for example, only 3% of kidneys transplanted during 2006 in Spain came from living donors.[xv] In Spain all citizens are potential organ donors in the case of their death, unless they explicitly opt out during their lifetime.[16]
Living donors [edit]
Approximately one in iii donations in the Us, Britain, and Israel is now from a live donor.[17] [18] [nineteen] Potential donors are advisedly evaluated on medical and psychological grounds. This ensures that the donor is fit for surgery and has no disease which brings undue gamble or likelihood of a poor outcome for either the donor or recipient. The psychological assessment is to ensure the donor gives informed consent and is not coerced. In countries where paying for organs is illegal, the authorities may also seek to ensure that a donation has not resulted from a financial transaction.

Kidney for transplant from live donor
The human relationship the donor has to the recipient has evolved over the years. In the 1950s, the start successful living donor transplants were betwixt identical twins. In the 1960s–1970s, live donors were genetically related to the recipient. However, during the 1980s–1990s, the donor pool was expanded farther to emotionally related individuals (spouses, friends). Now the elasticity of the donor relationship has been stretched to include acquaintances and even strangers ('donating donors'). In 2009, US transplant recipient Chris Strouth received a kidney from a donor who continued with him on Twitter, which is believed to be the first such transplant bundled entirely through social networking.[xx] [21]
Exchanges and chains are a novel arroyo to expand the living donor pool. In February 2012, this novel approach to aggrandize the living donor pool resulted in the largest concatenation in the globe, involving 60 participants organized by the National Kidney Registry.[22] In 2014 the record for the largest chain was broken again by a swap involving 70 participants.[23] The acceptance of altruistic donors has enabled chains of transplants to form. Kidney chains are initiated when an altruistic donor donates a kidney to a patient who has a willing only incompatible donor. This incompatible donor then 'pays it forrad' and passes on the generosity to some other recipient who as well had a willing but incompatible donor. Michael Rees from the University of Toledo developed the concept of open up-ended chains.[24] This was a variation of a concept developed at Johns Hopkins University.[25] On thirty July 2008, an altruistic donor kidney was shipped via commercial airline from Cornell to UCLA, thus triggering a concatenation of transplants.[26] The shipment of living donor kidneys, computer-matching software algorithms, and cooperation between transplant centers has enabled long-elaborate chains to be formed.[27]
In 2004 the FDA canonical the Cedars-Sinai High Dose IVIG therapy which reduces the need for the living donor to be the aforementioned blood blazon (ABO compatible) or even a tissue match.[28] [29] The therapy reduced the incidence of the recipient'due south immune system rejecting the donated kidney in highly sensitized patients.[29]
In advisedly screened kidney donors, survival and the risk of end-stage renal affliction appear to exist similar to those in the general population.[xxx] However, some more recent studies suggest that lifelong take a chance of chronic kidney disease is several-fold higher in kidney donors although the absolute take a chance is nonetheless very minor.[31]
A 2017 article in the New England Journal of Medicine suggests that persons with just one kidney, including those who have donated a kidney for transplantation, should avoid a high protein diet and limit their protein intake to less than ane gram per kilogram body weight per day in order to reduce the long-term take chances of chronic kidney affliction.[32] Women who have donated a kidney have a higher risk of gestational hypertension and preeclampsia than matched nondonors with similar indicators of baseline health.[33]
Surgical procedure [edit]
Traditionally, the donor process has been through a unmarried incision of 4–7 inches (10–18 cm), but live donation is being increasingly performed by laparoscopic surgery. This reduces pain and accelerates recovery for the donor. Operative time and complications decreased significantly after a surgeon performed 150 cases. Live donor kidney grafts have college long-term success rates than those from deceased donors.[34] Since the increment in the use of laparoscopic surgery, the number of alive donors has increased. Any advance which leads to a decrease in pain and scarring and swifter recovery has the potential to heave donor numbers. In January 2009, the outset all-robotic kidney transplant was performed at Saint Barnabas Medical Center, located in Livingston, New Jersey, through a two-inch incision. In the following six months, the same squad performed 8 more robotic-assisted transplants.[35]
In 2009 at the Johns Hopkins Medical Center, a healthy kidney was removed through the donor's vagina. Vaginal donations promise to speed recovery and reduce scarring.[36] The first donor was called as she had previously had a hysterectomy.[37] The extraction was performed using natural orifice transluminal endoscopic surgery, where an endoscope is inserted through an orifice, then through an internal incision, so that there is no external scar. The contempo accelerate of single port laparoscopy requiring only one entry point at the navel is another advance with potential for more frequent utilize.
Organ merchandise [edit]
In the developing world some people sell their organs illegally. Such people are often in grave poverty[38] or are exploited by salespersons. The people who travel to make use of these kidneys are often known as 'transplant tourists'. This practise is opposed past a variety of homo rights groups, including Organs Watch, a group established past medical anthropologists, which was instrumental in exposing illegal international organ selling rings. These patients may have increased complications owing to poor infection command and lower medical and surgical standards. One surgeon has said that organ trade could be legalised in the Britain to prevent such tourism, simply this is not seen by the National Kidney Research Fund as the respond to a arrears in donors.[39]
In the illegal blackness market the donors may not get sufficient after-performance intendance,[40] the price of a kidney may be in a higher place $160,000,[41] middlemen have almost of the money, the performance is more dangerous to both the donor and receiver, and the heir-apparent oft gets hepatitis or HIV.[42] In legal markets of Iran the price of a kidney is $ii,000 to $4,000.[42] [43]
An article by Gary Becker and Julio Elias on "Introducing Incentives in the market place for Live and Cadaveric Organ Donations"[44] said that a costless market could help solve the problem of a scarcity in organ transplants. Their economic modeling was able to estimate the cost tag for human kidneys ($15,000) and human livers ($32,000).
Jason Brennan and Peter Jaworski from Georgetown Academy have also argued that whatsoever moral objections to a market for organs are not inherent in the marketplace, but rather the activity itself.[45]
Monetary compensation for organ donors, in the course of reimbursement for out-of-pocket expenses, has been legalised in Commonwealth of australia and Singapore.[46] [47] [48]
Donors [edit]
Deceased donors [edit]

Kidney donor cards from England, 1971–1981. The cards were made to be carried by donors equally prove that they were willing to donate their kidneys should they, for example, be killed in an accident.
Deceased donors can be divided in ii groups:
- Encephalon-dead (BD) donors
- Donation after Cardiac Death (DCD) donors
Although brain-dead (or 'center beating') donors are considered dead, the donor'due south heart continues to pump and maintain circulation. This makes it possible for surgeons to outset operating while the organs are still existence perfused (supplied blood). During the operation, the aorta will exist cannulated, after which the donor'south blood volition be replaced by an water ice-cold storage solution, such as UW (Viaspan), HTK, or Perfadex. Depending on which organs are transplanted, more than i solution may be used simultaneously. Due to the temperature of the solution, and since large amounts of cold NaCl-solution are poured over the organs for a rapid cooling, the heart will stop pumping.
'Donation after Cardiac Death' donors are patients who do non see the encephalon-dead criteria only, due to the unlikely chance of recovery, have elected via a living volition or through family unit to accept support withdrawn. In this procedure, treatment is discontinued (mechanical ventilation is close off). Later a fourth dimension of death has been pronounced, the patient is rushed to the operating room where the organs are recovered. Storage solution is flushed through the organs. Since the blood is no longer being circulated, coagulation must exist prevented with large amounts of anti-coagulation agents such as heparin. Several ethical and procedural guidelines must exist followed; near importantly, the organ recovery team should non participate in the patient's intendance in any manner until after expiry has been alleged.
Increased donors [edit]
Many governments have passed laws whereby the default is an opt-in organisation in order to increase the number of donors.
Since December 2015, Human Transplantation (Wales) Human activity 2013 passed by the Welsh Government has enabled an opt-out organ donation register, the first country in the UK to practise and so. The legislation is 'deemed consent', whereby all citizens are considered to take no objection to becoming a donor unless they accept opted out on this register.[49]
Animal transplants [edit]
In 2022, University of Alabama Birmingham announced the first peer-reviewed research outlining the successful transplant of genetically modified, clinical-grade grunter kidneys into a brain-expressionless human individual, replacing the recipient'due south native kidneys. In the study, which was published in the American Journal of Transplantation, researchers tested the first human preclinical model for transplanting genetically modified pig kidneys into humans. The recipient of the study had his native kidneys removed and received two genetically modified pig kidneys in their identify. The organs came from a genetically-modified sus scrofa from a pathogen-gratis facility.[50]
Compatibility [edit]
In general, the donor and recipient should be ABO claret group and crossmatch (human leukocyte antigen – HLA) uniform. If a potential living donor is incompatible with their recipient, the donor could exist exchanged for a uniform kidney. Kidney commutation, likewise known every bit "kidney paired donation" or "chains" have recently gained popularity.[ citation needed ]
In an effort to reduce the risk of rejection during incompatible transplantation, ABO-incompatible and desensitization protocols utilizing intravenous immunoglobulin (IVIG) take been developed, with the aim to reduce ABO and HLA antibodies that the recipient may have to the donor. In 2004 the FDA approved the Cedars-Sinai High Dose IVIG therapy which reduces the need for the living donor to be the same claret type (ABO compatible) or even a tissue match.[51] [29] The therapy reduced the incidence of the recipient'due south immune organisation rejecting the donated kidney in highly sensitized patients.[29]
In the 1980s, experimental protocols were developed for ABO-incompatible transplants using increased immunosuppression and plasmapheresis. Through the 1990s these techniques were improved and an important written report of long-term outcomes in Nippon was published.[52] At present, a number of programs effectually the globe are routinely performing ABO-incompatible transplants.[53]
The level of sensitization to donor HLA antigens is determined by performing a panel reactive antibody test on the potential recipient. In the United States, up to 17% of all deceased donor kidney transplants have no HLA mismatch. Still, HLA matching is a relatively small predictor of transplant outcomes. In fact, living not-related donors are now almost as mutual as living (genetically)-related donors.[ citation needed ]
Procedure [edit]

In near cases the barely functioning existing kidneys are not removed, every bit removal has been shown to increase the rates of surgical morbidity. Therefore, the kidney is usually placed in a location dissimilar from the original kidney. Ofttimes this is in the iliac fossa so it is often necessary to apply a different blood supply:
- The renal artery of the new kidney, previously branching from the abdominal aorta in the donor, is ofttimes connected to the external iliac artery in the recipient.
- The renal vein of the new kidney, previously draining to the junior vena cava in the donor, is often continued to the external iliac vein in the recipient.
The donor ureter is anastomosed with the recipient bladder. In some cases a ureteral stent is placed at the time of the anastomosis, with the assumption that it allows for better drainage and healing. Still, using a modified Lich-Gregoir technique, Gaetano Ciancio developed a technique which no longer requires ureteral stenting, avoiding many stent related complications.[54]
At that place is disagreement in surgical textbooks regarding which side of the recipient's pelvis to use in receiving the transplant. Campbell'southward Urology (2002) recommends placing the donor kidney in the recipient's contralateral side (i.e. a left sided kidney would be transplanted in the recipient's right side) to ensure the renal pelvis and ureter are anterior in the upshot that future surgeries are required. In an instance where at that place is doubt over whether there is enough space in the recipient's pelvis for the donor's kidney, the textbook recommends using the correct side because the right side has a wider pick of arteries and veins for reconstruction.
Glen'south Urological Surgery (2004) recommends putting the kidney in the contralateral side in all circumstances. No reason is explicitly put forth; however, one can assume the rationale is like to that of Campbell, i.e. to ensure that the renal pelvis and ureter are most anterior in the issue that hereafter surgical correction becomes necessary.
Smith's Urology (2004) states that either side of the recipient's pelvis is adequate; even so the right vessels are 'more than horizontal' with respect to each other and therefore easier to employ in the anastomoses. Information technology is unclear what is meant by the words 'more horizontal'.
Kidney-pancreas transplant [edit]
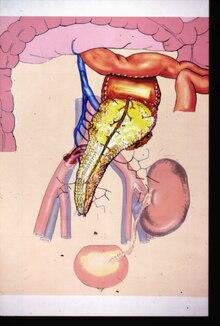
Kidney-pancreas transplant
Occasionally, the kidney is transplanted together with the pancreas. Academy of Minnesota surgeons Richard Lillehei and William Kelly perform the showtime successful simultaneous pancreas-kidney transplant in the world in 1966.[55] This is done in patients with diabetes mellitus type i, in whom the diabetes is due to destruction of the beta cells of the pancreas and in whom the diabetes has caused kidney failure (diabetic nephropathy). This is most always a deceased donor transplant. Only a few living donor (partial) pancreas transplants have been done. For individuals with diabetes and kidney failure, the advantages of an before transplant from a living donor (if available) are far superior to the risks of continued dialysis until a combined kidney and pancreas are available from a deceased donor.[ citation needed ] A patient tin can either receive a living kidney followed by a donor pancreas at a later on appointment (PAK, or pancreas-afterward-kidney) or a combined kidney-pancreas from a donor (SKP, simultaneous kidney-pancreas).
Transplanting just the islet cells from the pancreas is still in the experimental stage but shows promise. This involves taking a deceased donor pancreas, breaking it downwardly, and extracting the islet cells that make insulin. The cells are then injected through a catheter into the recipient and they generally guild in the liver. The recipient still needs to have immunosuppressants to avert rejection, but no surgery is required. Most people need 2 or three such injections, and many are not completely insulin-free.
Mail operation [edit]
The transplant surgery takes nigh three hours.[56] The donor kidney will be placed in the lower belly and its blood vessels continued to arteries and veins in the recipient's torso. When this is consummate, blood will be immune to flow through the kidney once more. The terminal step is connecting the ureter from the donor kidney to the bladder. In most cases, the kidney will before long starting time producing urine.
Depending on its quality, the new kidney normally begins functioning immediately. Living donor kidneys commonly crave 3–5 days to reach normal functioning levels, while cadaveric donations stretch that interval to 7–fifteen days. Hospital stay is typically for 4–ten days. If complications arise, additional medications (diuretics) may be administered to help the kidney produce urine.
Immunosuppressant drugs are used to suppress the immune organization from rejecting the donor kidney. These medicines must exist taken for the rest of the recipient'due south life. The most common medication regimen today is a mixture of tacrolimus, mycophenolate, and prednisolone. Some recipients may instead take ciclosporin, sirolimus, or azathioprine. The risk of early rejection of the transplanted kidney is increased if corticosteroids are avoided or withdrawn after the transplantation.[57] Ciclosporin, considered a breakthrough immunosuppressive when first discovered in the 1980s, ironically causes nephrotoxicity and tin can result in iatrogenic damage to the newly transplanted kidney. Tacrolimus, which is a similar drug, also causes nephrotoxicity. Blood levels of both must be monitored closely and if the recipient seems to accept declining kidney function or proteinuria, a kidney transplant biopsy may be necessary to determine whether this is due to rejection [58] [59] or ciclosporin or tacrolimus intoxication .
Imaging [edit]
Postal service operatively, kidneys are periodically assessed by ultrasound to assess for the imaging and physiologic changes that accompany transplant rejection. Imaging besides allows evaluation of supportive structures such equally the anastomosed transplant avenue, vein, and ureter, to ensure they are stable in advent.
The major sonographic scale in quantitative ultrasound assessment is with a multipoint assessment of the resistive index (RI), offset at the primary renal artery and vein and ending at the arcuate vessels. Information technology is calculated as follows:
- RI = (peak systolic velocity – stop diastolic velocity ) / peak systolic velocity
The normal value is ≈ 0.60, with 0.seventy being the upper limits of normal.[60] [61]
Mail service-transplantation radioisotope renography tin can exist used for the diagnosis of vascular and urological complications.[62] Also, early post-transplantation renography is used for the cess of delayed graft function.[63] [64]
Diet [edit]
Kidney transplant recipients are discouraged from consuming grapefruit, pomegranate and dark-green tea products. These food products are known to collaborate with the transplant medications, specifically tacrolimus, cyclosporin and sirolimus; the blood levels of these drugs may be increased, potentially leading to an overdose.[65]
Astute rejection occurs in 10–25% of people later on transplant during the get-go 60 days.[ citation needed ] Rejection does non necessarily hateful loss of the organ, merely it may necessitate additional handling and medication adjustments.[66]
Complications [edit]
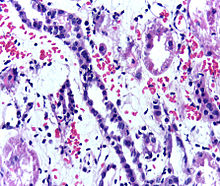
Presence of lymphocytes within the tubular epithelium, attesting to astute cellular rejection of a renal graft. Biopsy sample.
Bug later on a transplant may include:
- Post operative complications, such as bleeding, infection, vascular thrombosis and urinary complications[67]
- Transplant rejection (hyperacute, acute or chronic)[67]
- Infections and sepsis due to the immunosuppressant drugs that are required to decrease run a risk of rejection [68]
- Postal service-transplant lymphoproliferative disorder (a form of lymphoma due to the immune suppressants). This occurs in about ii% of patients, occurring specially in the outset ii years post-transplant[67]
- Pare tumours[69]
- Imbalances in electrolytes including calcium and phosphate which tin lead to bone problems
- Proteinuria[59]
- Hypertension
- Recurrence of original cause of kidney failure
- Other side effects of medications including gastrointestinal inflammation and ulceration of the stomach and esophagus, hirsutism (excessive hair growth in a male-design distribution) with ciclosporin, hair loss with tacrolimus, obesity, acne, diabetes mellitus type 2, hypercholesterolemia, and osteoporosis.
A patient'due south historic period and health condition earlier transplantation touch on the risk of complications. Dissimilar transplant centers take different success at managing complications; and therefore, complication rates are dissimilar from middle to centre.
The boilerplate lifetime for a kidney from a deceased donor is 10 years, and fifteen years for a kidney from a living donor. When a transplant fails, a patient may opt for a 2d transplant, or may accept to return to dialysis for some intermediary fourth dimension. A few (usually older) patients choose not to render to dialysis and be treated with supportive intendance (no dialysis or transplant).
Infections due to the immunosuppressant drugs used in people with kidney transplants nigh unremarkably occur in mucocutaneous areas (41%), the urinary tract (17%) and the respiratory tract (xiv%).[70] The nigh common infective agents are bacterial (46%), viral (41%), fungal (thirteen%), and protozoan (one%).[70] Of the viral illnesses, the nigh common agents are human cytomegalovirus (31.5%), canker simplex (23.4%), and herpes zoster (23.4%).[70] BK virus is now existence increasingly recognised equally a transplant risk factor.[71] Infection is the cause of decease in almost 1 third of people with renal transplants, and pneumonias business relationship for 50% of the patient deaths from infection.[70]
-
Postoperative bleeding following kidney transplant as seen on ultrasound[72]
-
Postoperative bleeding post-obit kidney transplant every bit seen on ultrasound[72]
-
Postoperative bleeding following kidney transplant as seen on ultrasound[72]
-

Postoperative haemorrhage following kidney transplant every bit seen on ultrasound[72]
Prognosis [edit]
Kidney transplantation is a life-extending procedure.[73] The typical patient will live x to 15 years longer with a kidney transplant than if kept on dialysis.[74] The increment in longevity is greater for younger patients, but even 75-year-old recipients (the oldest grouping for which at that place is data) gain an average four more years of life. People generally have more energy, a less-restricted nutrition, and fewer complications with a kidney transplant than if they stay on conventional dialysis.[ commendation needed ]
Some studies seem to suggest that the longer a patient is on dialysis earlier the transplant, the less fourth dimension the kidney will last. Information technology is not clear why this occurs, simply it underscores the need for rapid referral to a transplant program. Ideally, a kidney transplant should be pre-emptive, i.e., take identify before the patient begins dialysis. The reason why kidneys fail over time after transplantation has been elucidated in recent years. Autonomously from recurrence of the original kidney affliction, rejection (mainly antibody-mediated rejection) and progressive scarring (multifactorial) besides play a decisive role.[75] Fugitive rejection by strict medication adherence is of utmost importance to avoid failure of the kidney transplant.[ citation needed ]
At least 4 professional person athletes have made a comeback to their sport after receiving a transplant: New Zealand rugby union role player Jonah Lomu, German-Croatian soccer role player Ivan Klasnić, and NBA basketballers Sean Elliott and Alonzo Mourning.[ citation needed ]
For live kidney donors, prognostic studies are potentially confounded a selection bias wherein kidney donors are selected among people who are healthier than the general population, only when matching to a respective healthy control grouping, there appears to be no deviation in overall long-term mortality rates amid kidney donors.[76]
Statistics [edit]
| Country | Year | Cadaveric donor | Living donor | Total transplants |
|---|---|---|---|---|
| Commonwealth of australia[77] [78] | 2020 | 704 | 182 | 886 |
| Canada[79] | 2020 | one,063 | 396 | 1,459 |
| France[80] | 2003 | ane,991 | 136 | ii,127 |
| Italy[80] | 2003 | ane,489 | 135 | ane,624 |
| Japan[81] | 2010 | 208 | 1276 | 1,484 |
| Spain[80] | 2003 | 1,991 | sixty | two,051 |
| United Kingdom[80] | April 2020 to March 2021 | i,836 | 422 | ii,258 |
| United States[82] | 2020 | 17,583 | 5,234 | 22,817 |
In add-on to nationality, transplantation rates differ based on race, sexual practice, and income. A report washed with patients beginning long-term dialysis showed that the socio-demographic barriers to renal transplantation are relevant fifty-fifty earlier patients are on the transplant list.[83] For example, different socio-demographic groups express dissimilar involvement and complete pre-transplant workup at unlike rates. Previous efforts to create off-white transplantation policies have focused on patients currently on the transplantation waiting list.
In the U.South. health system [edit]
Transplant recipients must take immunosuppressive anti-rejection drugs for as long as the transplanted kidney functions. The routine immunosuppressives are tacrolimus (Prograf), mycophenolate (Cellcept), and prednisolone; these drugs toll US$1,500 per month. In 1999 the United states of america Congress passed a constabulary that restricts Medicare from paying for more than three years for these drugs unless the patient is otherwise Medicare-eligible. Transplant programs may not transplant a patient unless the patient has a reasonable plan to pay for medication later on Medicare coverage expires; notwithstanding, patients are virtually never turned down for fiscal reasons solitary. One-half of end-stage renal disease patients simply accept Medicare coverage. This provision was repealed in December 2020; the repeal volition come into effect on January 1st 2023. People who were on Medicare, or who had applied for Medicare at the time of their procedure, will accept lifetime coverage of post-transplant drugs.[84]
The United Network for Organ Sharing, which oversees the organ transplants in the U.s.a., allows transplant candidates to annals at two or more transplant centers, a practice known as 'multiple list'.[85] The practice has been shown to be effective in mitigating the dramatic geographic disparity in the waiting fourth dimension for organ transplants,[86] especially for patients residing in loftier-demand regions such as Boston.[87] The practice of multiple-listing has likewise been endorsed past medical practitioners.[88] [89]
Notable recipients [edit]
Run across too Category:Kidney transplant recipients and Listing of organ transplant donors and recipients
- Steven Cojocaru (born 1970), Canadian fashion critic, transplants in ???? and 2005
- Andy Cole (born 1971), English footballer, transplant in Apr 2017 [ninety] [91] [92]
- Natalie Cole (1950–2015), American vocaliser, transplant in 2009 (survival: half dozen years)
- Gary Coleman (1968–2010), American actor, outset transplant <5 years old, 2nd transplant at 14 years sometime (circa 1981) [93]
- Lucy Davis (born 1973), English actress, transplant in 1997
- Kenny Easley (born 1959), American football actor, transplant in 1990
- Aron Eisenberg (1969-2019), American histrion, transplant in 1986 and 2015 (survival 23 and 4 years)
- David Ayres (built-in 1977), Canadian Hockey Player, transplant in 2004
- Sean Elliott (born 1968), American basketball actor, transplant in 1999
- Selena Gomez (born 1992), American singer, songwriter and extra, transplant in 2017
- Jennifer Harman (born 1964), American poker player, transplants in ???? and 2004
- Ken Howard (born 1932), English creative person, transplant in 2000
- Sarah Hyland (born 1990), American actress, transplant in 2012
- Ivan Klasnić (born 1980), Croation footballer, transplant in 2007
- Jimmy Little (1937–2012), Australian musician and actor, transplant in 2004 (survival: 8 years)
- Jonah Lomu (1975–2015), New Zealand rugby player, transplant in 2004 (survival: 11 years)
- George Lopez (born 1961), American comedian and histrion, transplant in 2005
- Tracy Morgan (built-in 1968), American comedian and actor, transplant in 2010
- Alonzo Mourning (born 1970), American basketball player, transplant in 2003
- Kerry Packer (1937–2005), Australian businessman, transplant in 2000 (survival: 5 years)
- Charles Perkins (1936–2000), Australian footballer and activist, transplant in 1972 (survival: 28 years)
- Baton Preston (1946–2006), American musician, transplant in 2002 (survival: 4 years)
- Neil Simon (1927–2018), American playwright, transplant in 2004 (survival: 14 years)
- Ron Springs (1956–2011), American football game player, transplant in 2007 (survival: iv years) [ citation needed ]
- Tomomi "Jumbo" Tsuruta (1951–2000), Japanese professional wrestler, transplant in 2000 (survival: one month)
- Elliot F. Kaye, American lawyer, chairman of the U.S. Consumer Production Rubber Commission, transplant in 2022 [94]
See too [edit]
- Artificial kidney
- Gurgaon kidney scandal
- Jesus Christians – an Australian religious group, many of whose members have donated a kidney to a stranger
- Liver transplantation
Bibliography [edit]
- Brook, Nicholas R.; Nicholson, Michael L. (2003). "Kidney transplantation from not centre-beating donors". Surgeon. 1 (6): 311–322. doi:10.1016/S1479-666X(03)80065-3. PMID 15570790.
- Danovitch, Gabriel M.; Delmonico, Francis L. (2008). "The prohibition of kidney sales and organ markets should remain". Electric current Opinion in Organ Transplantation. 13 (iv): 386–394. doi:10.1097/MOT.0b013e3283097476. PMID 18685334.
- El-Agroudy, Amgad Eastward.; El-Husseini, Amr A.; El-Sayed, Moharam; Ghoneim, Mohamed A. (2003). "Preventing Bone Loss in Renal Transplant Recipients with Vitamin D". Journal of the American Society of Nephrology. xiv (11): 2975–2979. doi:10.1097/01.ASN.0000093255.56474.B4. PMID 14569109.
- El-Agroudy, Amgad Eastward.; Sabry, Alaa A.; Wafa, Ehab W.; Neamatalla, Ahmed H.; Ismail, Amani One thousand.; Mohsen, Tarek; Khalil, Abd Allah; Shokeir, Ahmed A.; Ghoneim, Mohamed A. (2007). "Long-term follow-up of living kidney donors: a longitudinal study". BJU International. 100 (6): 1351–1355. doi:ten.1111/j.1464-410X.2007.07054.x. ISSN 1464-4096. PMID 17941927. S2CID 32904086. [ dead link ]
- Grens, Kerry (9 April 2012). "Living kidney donations favor some patient groups: written report". Reuters.
- Gore John L, et al. (2012). "The Socioeconomic Status of Donors and Recipients of Living Unrelated Renal Transplants in the United States". The Journal of Urology. 187 (5): 1760–1765. doi:10.1016/j.juro.2011.12.112. PMID 22425125.
Notes [edit]
- ^ a b c d "20 Mutual Kidney Transplant Questions and Answers". National Kidney Foundation. 26 January 2017. Archived from the original on 21 March 2021. Retrieved 23 March 2021.
- ^ "The Kidney Transplant Waitlist – What You Demand to Know". National Kidney Foundation. x February 2017. Retrieved 26 March 2021.
- ^ a b c Voora S, Adey DB (June 2019). "Management of Kidney Transplant Recipients by General Nephrologists: Core Curriculum 2019". American Journal of Kidney Diseases. 73 (six): 866–879. doi:x.1053/j.ajkd.2019.01.031. PMID 30981567.
- ^ "International Report on Organ Donation And Transplantation Activities: Executive Summary 2018" (PDF). Global Observatory on Donation and Transplantation. ONT/WHO. Oct 2020. Archived (PDF) from the original on 21 March 2021. Retrieved 24 March 2021.
- ^ Shrestha B, Haylor J, Raftery A (March 2015). "Historical Perspectives in Kidney Transplantation: An Updated Review". Progress in Transplantation. 25 (i): 64–69. doi:10.7182/pit2015789. PMID 25758803. S2CID 26032497.
- ^ MAY TRANSPLANT THE Homo HEART (.PDF), The New York Times, 2 January 1908
- ^ Matevossian E, Kern H, Hüser Due north, Doll D, Snopok Y, Nährig J, Altomonte J, Sinicina I, Friess H, Thorban Southward (Dec 2009). "Surgeon Yurii Voronoy (1895–1961) – a pioneer in the history of clinical transplantation: in Memoriam at the 75th Anniversary of the Starting time Man Kidney Transplantation". Transplant International. 22 (12): 1132–1139. doi:10.1111/j.1432-2277.2009.00986.x. PMID 19874569. S2CID 12087935.
- ^ Stressmarq.com; Indiatoday.intoday.in; Healthcentral.com (retrieved 12 February 2018)
- ^ David Petechuk (2006). Organ transplantation . Greenwood Publishing Group. p. 11. ISBN978-0-313-33542-6.
- ^ Legendre, Ch; Kreis, H. (November 2010). "A Tribute to Jean Hamburger'southward Contribution to Organ Transplantation". American Periodical of Transplantation. 10 (11): 2392–2395. doi:10.1111/j.1600-6143.2010.03295.x. PMID 20977631. S2CID 24674177.
- ^ "Transplant Pioneers Recall Medical Milestone". NPR. twenty December 2004. Retrieved 20 December 2010.
- ^ Hakim, Nadey (2010). Living Related Transplantation. World Scientific. p. 39. ISBN978-1-84816-497-0.
- ^ Daar, Abdallah S.; Al Lawati, Nabil Mohsin (December ane, 2016). "The World's Youngest Cadaveric Kidney Transplant: Medical, Surgical and Ethical Issues". Transplant Straight. 2 (12 (Article number: e117)): e117. doi:ten.1097/TXD.0000000000000631. ISSN 2373-8731. OCLC 8892768132. PMC5142357. PMID 27990482.
- ^ Organ Procurement and Transplantation Network, 2007
- ^ Organización Nacional de Transplantes (ONT), 2007
- ^ "How Spain became the globe leader in organ transplants". The Local. 15 September 2017.
- ^ "How to become an organ donor". The Sentry. 24 Feb 2009. Retrieved 19 Dec 2010.
- ^ HighBeam Judy Siegel, "Live liver and lung donations approved. New regulations will give hope to dozens." 'Jerusalem Post', ix May 1995 "(subscription required)
- ^ "National Data Reports". The Organ Procurement and Transplant Network (OPTN). dynamic. Retrieved 22 October 2013. (the link is to a query interface; Choose Category = Transplant, Organ = Kidney, and select the 'Transplant by donor type' report link)
- ^ Kiser, Kim (August 2010). "More than than Friends and Followers: Facebook, Twitter, and other forms of social media are connecting organ recipients with donors". Minnesota Medicine. Retrieved 17 October 2014.
- ^ "To Share or Not to Share on Social Media". The Ricki Lake Show. Season 1. Episode 19. 4 October 2014. Issue occurs at 29:40. 20th Television. Archived from the original on 2013-08-03. Retrieved 17 October 2014.
- ^ Sack, Kevin (xviii February 2012). "lx Lives, 30 Kidneys, All Linked". New York Times.
- ^ Pitts, Byron (15 April 2015). "Changing Lives Through Donating Kidneys to Strangers". ABC News Nightline.
- ^ Rees Chiliad. A.; Kopke J. E.; Pelletier R. P.; Segev D. L.; Rutter Chiliad. Due east.; Fabrega A. J.; et al. (2009). "A nonsimultaneous, extended, donating-donor chain". The New England Journal of Medicine. 360 (11): 1096–1101. doi:10.1056/NEJMoa0803645. PMID 19279341.
- ^ Montgomery R. A.; Gentry Southward. E.; Marks West. H.; Warren D. Southward.; Hiller J.; Houp J.; et al. (2006). "Domino paired kidney donation: a strategy to make best use of alive non-directed donation". Lancet. 368 (9533): 419–421. CiteSeerX10.1.1.576.6386. doi:10.1016/S0140-6736(06)69115-0. PMID 16876670. S2CID 2035816.
- ^ Butt F. Thou.; Gritsch H. A.; Schulam P.; Danovitch G. M.; Wilkinson A.; Del Pizzo J.; et al. (2009). "Asynchronous, Out-of-Sequence, Transcontinental Chain Kidney Transplantation: A Novel Concept". American Journal of Transplantation. 9 (9): 2180–2185. doi:10.1111/j.1600-6143.2009.02730.ten. PMID 19563335. S2CID 26186779.
- ^ Sack, Kevin. (19 February 2012). "60 Lives, 30 Kidneys, All Linked". The New York Times . Retrieved 22 October 2013.
- ^ "Kidney and Pancreas Transplant Center – ABO Incompatibility". Cedars-Sinai Medical Centre. Retrieved 12 October 2009.
- ^ a b c d Jordan SC, Tyan D, Stablein D, et al. (December 2004). "Evaluation of intravenous immunoglobulin as an agent to lower allosensitization and improve transplantation in highly sensitized adult patients with end-phase renal disease: report of the NIH IG02 trial". J Am Soc Nephrol. 15 (12): 3256–62. doi:10.1097/01.ASN.0000145878.92906.9F. PMID 15579530.
- ^ Ibrahim, H. N.; Foley, R; Tan, L; Rogers, T; Bailey, RF; Guo, H; Gross, CR; Matas, AJ (2009). "Long-Term Consequences of Kidney Donation". Northward Engl J Med. 360 (five): 459–46. doi:x.1056/NEJMoa0804883. PMC3559132. PMID 19179315.
- ^ Muzaale AD, Massie AB, Wang MC, Montgomery RA, McBride MA, Wainright JL, Segev DL (12 February 2014). "Hazard of terminate-stage renal affliction post-obit live kidney donation". JAMA. 311 (half dozen): 579–86. doi:ten.1001/jama.2013.285141. PMC4411956. PMID 24519297.
- ^ Kalantar-Zadeh 1000, Fouque D (two November 2017). "Nutritional direction of chronic kidney disease". N. Engl. J. Med. 377 (xviii): 1765–1776. doi:10.1056/NEJMra1700312. PMID 29091561. S2CID 27499763.
- ^ Garg, Amit X.; Nevis, Immaculate F.; McArthur, Eric; Sontrop, Jessica M.; Koval, John J.; Lam, Ngan North.; Hildebrand, Ainslie Yard.; Reese, Peter P.; Storsley, Leroy; Gill, John Due south.; Segev, Dorry L.; Habbous, Steven; Bugeja, Ann; Knoll, Greg A.; Dipchand, Christine; Monroy-Cuadros, Mauricio; Lentine, Krista L. (2014). "Gestational Hypertension and Preeclampsia in Living Kidney Donors". New England Journal of Medicine. 372 (2): 124–133. doi:10.1056/NEJMoa1408932. ISSN 0028-4793. PMC4362716. PMID 25397608.
- ^ "Kidney Transplant". National Health Service. 29 March 2010. Retrieved 19 November 2011.
- ^ New Robot Engineering Eases Kidney Transplants Archived 4 August 2009 at the Wayback Machine, CBS News, 22 June 2009 – accessed viii July 2009
- ^ "Donor kidney removed via vagina". BBC News. 3 February 2009. Retrieved 12 October 2009.
- ^ "Surgeons remove healthy kidney through donor's vagina - CNN.com". cnn.com. 3 February 2009. Retrieved 12 October 2009.
- ^ Rohter, Larry (23 May 2004). "The Organ Trade – A Global Black Market – Tracking the Sale of a Kidney On a Path of Poverty and Hope". New York Times . Retrieved 19 December 2010.
- ^ "Call to legalise live organ trade". 19 May 2003 – via news.bbc.co.united kingdom of great britain and northern ireland.
- ^ The Meat Market, The Wall Street Journal, 8 January 2010.
- ^ Martinez, Edecio (27 July 2009). "Black Market place Kidneys, $160,000 a Popular". CBS News. Archived from the original on 4 November 2012. Retrieved 12 June 2011.
- ^ a b "Psst, wanna purchase a kidney?". Organ transplants. The Economist Newspaper Express 2011. 16 November 2006. Retrieved 12 June 2011.
- ^ Schall, John A. (May 2008). "A New Outlook on Compensated Kidney Donations". RENALIFE. American Association of Kidney Patients. Archived from the original on 27 September 2011. Retrieved 14 June 2011.
- ^ Gary S. Becker; Julio Jorge Elías. "Introducing Incentives in the Market for Live and Cadaveric Organ Donations" (PDF). New York Times . Retrieved 24 December 2013.
- ^
- ^ Plibersek, Tanya (7 April 2013). "Supporting Paid Exit for Living Organ Donors". Retrieved 18 Baronial 2021.
- ^ Bland, B (2008). "Singapore legalises bounty payments to kidney donors". BMJ. 337: a2456. doi:10.1136/bmj.a2456. PMID 18996933. S2CID 38062784.
- ^ "Singapore: Homo Organ Transplant Act Amended". Library of Congress. xv Apr 2009. Retrieved 19 Baronial 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Organ donation police force in Wales". NHS Wales . Retrieved 31 January 2021.
- ^ Porrett, Paige M.; Orandi, Babak J.; Kumar, Vineeta; Houp, Julie; Anderson, Douglas; Killian, A. Cozette; Hauptfeld-Dolejsek, Vera; Martin, Dominique E.; Macedon, Sara; Budd, Natalie; Stegner, Katherine L. (2022). "Kickoff clinical-grade porcine kidney xenotransplant using a human decedent model". American Journal of Transplantation. n/a (north/a). doi:ten.1111/ajt.16930. ISSN 1600-6143. S2CID 246137465.
- ^ "Kidney and Pancreas Transplant Center – ABO Incompatibility". Cedars-Sinai Medical Center. Retrieved 12 October 2009.
- ^ "Archived copy" (PDF). Archived from the original (PDF) on 29 May 2008. Retrieved 4 May 2008.
{{cite spider web}}: CS1 maint: archived copy as title (link) - ^ "Overcoming Antibody Barriers to Kidney Transplant". discoverysedge.mayo.edu. Archived from the original on 28 August 2009. Retrieved 20 July 2009.
- ^ Gołębiewska, Justyna; Ciancio, Gaetano; Farag, Ahmed; Gonzalez, Javier; Vincenzi, Paolo; Gaynor, Jeffrey J. (2021). "Results of a previously unreported extravesical ureteroneocystostomy technique without ureteral stenting in 500 sequent kidney transplant recipients". PLOS 1. 16 (1): e0244248. Bibcode:2021PLoSO..1644248C. doi:10.1371/journal.pone.0244248. ISSN 1932-6203. PMC7799771. PMID 33428659.
- ^ David Eastward. R. Sutherland; Rainer West. M. Gruessner; David L. Dunn; Arthur J. Matas; Abhinav Humar; Raja Kandaswamy; S. Michael Mauer; William R. Kennedy; Frederick C. Goetz; R. Paul Robertson; Angelika C. Gruessner; John Southward. Najarian (April 2001). "Lessons Learned From More than Than one,000 Pancreas Transplants at a Single Institution". Ann. Surg. 233 (4): 463–501. doi:10.1097/00000658-200104000-00003. PMC1421277. PMID 11303130.
- ^ "Kidney transplant: MedlinePlus Medical Encyclopedia". National Institutes of Health. 22 June 2009. Retrieved xix December 2010.
- ^ Haller, Maria C.; Royuela, Ana; Nagler, Evi Five.; Pascual, Julio; Webster, Angela C. (22 Baronial 2016). "Steroid avoidance or withdrawal for kidney transplant recipients". The Cochrane Database of Systematic Reviews. 2016 (8): CD005632. doi:10.1002/14651858.CD005632.pub3. hdl:1854/LU-8083451. ISSN 1469-493X. PMC8520739. PMID 27546100.
- ^ Nankivell, B (2011). "Diagnosis and prevention of chronic kidney allograft loss". Lancet. 378 (9800): 1428–37. doi:ten.1016/s0140-6736(11)60699-5. PMID 22000139. S2CID 33946493.
- ^ a b Naesens (2015). "Proteinuria as a Noninvasive Marker for Renal Allograft Histology and Failure: An Observational Cohort Study". J Am Soc Nephrol. 27 (1): 281–92. doi:10.1681/ASN.2015010062. PMC4696583. PMID 26152270.
- ^ Krumme, B; Hollenbeck, Thousand (March 2007). "Doppler sonography in renal artery stenosis—does the Resistive Index predict the success of intervention?". Nephrology, Dialysis, Transplantation. 22 (three): 692–6. doi:10.1093/ndt/gfl686. PMID 17192278.
- ^ van de Kuit A, Benjamens Due south, Sotomayor CG, Rijkse E, Berger SP, Moers C, Bakker SJ, Minnee RC, Yakar D, Pol RA (2020). "Postoperative Ultrasound in Kidney Transplant Recipients: Association Betwixt Intrarenal Resistance Index and Cardiovascular Events". Transplant Straight. vi (eight): e581. doi:ten.1097/TXD.0000000000001034. PMC7581034. PMID 33134505.
- ^ Benjamens S, Berger SP, Glaudemans AW, Sanders JS, Politico RA, Slart RH (2018). "Renal scintigraphy for postal service-transplant monitoring afterwards kidney transplantation". Transplantation Reviews. 32 (two): 102–109. doi:10.1016/j.trre.2017.12.002. PMID 29395726.
- ^ Benjamens S, Political leader RA, de Geus-Oei LF, de Vries AP, Glaudemans AW, Berger SP, Slart RH (2018). "Can transplant renal scintigraphy predict the duration of delayed graft function? A dual center retrospective study". PLOS Ane. 13 (3): e0193791. Bibcode:2018PLoSO..1393791B. doi:10.1371/journal.pone.0193791. PMC5862448. PMID 29561854.
- ^ Benjamens S, Pol RA, Berger SP, Glaudemans AW, Dibbets-Schneider P, Slart RH, de Geus-Oei LF (2020). "Limited clinical value of two consecutive post-transplant renal scintigraphy procedures". European Radiology. 30 (i): 452–460. doi:10.1007/s00330-019-06334-1. PMC6890596. PMID 31338652.
- ^ "Transplant Medication Questions". Piedmont Hospital. 13 May 2011. Archived from the original on 17 September 2011. Retrieved 5 June 2011.
- ^ "Kidney transplant". www.webmd.com. Retrieved xx July 2009.
- ^ a b c Kim, Nancy; Juarez, Roxanna; Levy, Angela D. (October 2018). "Imaging non-vascular complications of renal transplantation". Abdominal Radiology. 43 (10): 2555–2563. doi:10.1007/s00261-018-1566-4. ISSN 2366-004X. PMID 29550956. S2CID 3969029.
- ^ Syu S-H, Lin Y-W, Lin One thousand-H, Lee L-M, Hsiao C-H, Wen Y-C. Run a risk factors for complications and graft failure in kidney transplant patients with sepsis. Bosn J of Basic Med Sci. 2019Aug.20;xix(3):304-11. A PMID: 30242808 PMCID: PMC6716102 DOI: 10.17305/bjbms.2018.3874
- ^ Roche CD, Dobson JS, Williams SK, Quante Thousand, Chow J (2014). "Cancerous and Noninvasive Peel Tumours in Renal Transplant Recipients". Dermatology Research and Practise. 409058: 409058. doi:10.1155/2014/409058. PMC4180396. PMID 25302063.
- ^ a b c d Renal Transplants > Renal Transplantation Complications from eMedicine. Author: Mert Erogul, MD; Chief Editor: Erik D Schraga, Doctor. Updated: 5 December 2008
- ^ Chong S, Antoni M, Macdonald A, Reeves M, Harber M, Magee CN (July 2019). "BK virus: Current understanding of pathogenicity and clinical affliction in transplantation" (PDF). Reviews in Medical Virology. 29 (four): e2044. doi:x.1002/rmv.2044. PMID 30958614. S2CID 102348985.
- ^ a b c d "UOTW #32 - Ultrasound of the Week". Ultrasound of the Week. eight January 2015. Retrieved 27 May 2017.
- ^ McDonald SP, Russ GR (2002). "Survival of recipients of cadaveric kidney transplants compared with those receiving dialysis treatment in Australia and New Zealand, 1991–2001". Nephrol. Dial. Transplant. 17 (12): 2212–9. doi:10.1093/ndt/17.12.2212. PMID 12454235.
- ^ Wolfe RA, Ashby VB, Milford EL, et al. (1999). "Comparison of Mortality in All Patients on Dialysis, Patients on Dialysis Awaiting Transplantation, and Recipients of a Get-go Cadaveric Transplant". NEJM. 341 (23): 1725–1730. doi:10.1056/nejm199912023412303. PMID 10580071. S2CID 1758680.
- ^ Naesens, M (2014). "The Histology of Kidney Transplant Failure: A Long-Term Follow-Up Study". Transplantation. 98 (4): 427–435. doi:10.1097/TP.0000000000000183. PMID 25243513. S2CID 20703626.
- ^ Morgan, Benjamin R.; Ibrahim, Hassan Due north. (2019). "Long-term outcomes of kidney donors". Arab Journal of Urology. 9 (ii): 79–84. doi:10.1016/j.aju.2011.06.006. ISSN 2090-598X. PMC4150560. PMID 26579273.
- ^ "2020 deceased organ donation and transplantation". DonateLife. 22 Feb 2021. Retrieved 19 August 2021.
{{cite web}}: CS1 maint: url-condition (link) - ^ "2020 living organ donation and transplantation". DonateLife. 22 February 2021. Retrieved 19 August 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "e-Statistics on organ transplants, waiting lists and donors | CIHI". www.cihi.ca . Retrieved 2021-08-xix .
- ^ a b c d "Transplant activity report". NHS Organ Donation . Retrieved 2021-08-19 .
- ^ "Kidney Transplantation Factbook 2011" (PDF).
- ^ "National Information Reports". The Organ Procurement and Transplant Network (OPTN). Retrieved 19 August 2021.
{{cite web}}: CS1 maint: url-status (link) (the link is to a query interface; Cull Category = Transplant, Organ = Kidney, and select the 'Transplant by donor type' study link) - ^ Alexander, G. C.; Sehgal, A. R. (1998). "Barriers to Cadaveric Renal Transplantation Amongst Blacks, Women, and the Poor". Journal of the American Medical Association. 280 (xiii): 1148–1152. doi:10.1001/jama.280.13.1148. PMID 9777814.
- ^ "Expanded Medicare Coverage of Immunosuppressive Drugs for Kidney Transplant Recipients". National Kidney Foundation. 2021-02-05. Retrieved 2021-05-27 .
- ^ "Questions & Answers for Transplant Candidates about Multiple Listing and Waiting Time Transfer" (PDF). United Network for Organ Sharing. Archived from the original (PDF) on 8 July 2014. Retrieved 6 March 2015.
- ^ Sommer Gentry (2013). "Addressing Geographic Disparities in Organ Availability" (PDF). Scientific Registry of Transplant Recipients (SRTR). Archived from the original (PDF) on September 4, 2014. Retrieved March half dozen, 2015.
- ^ Leamanczyk, Lauren (29 Nov 2014). "I-Team: Professor Helps Organ Transplant Patients On Multiple Waiting Lists". WBZ-TV. Retrieved thirty Nov 2014.
- ^ Ubel, P. A. (2014). "Transplantation Traffic — Geography as Destiny for Transplant Candidates". New England Journal of Medicine. 371 (26): 2450–2452. doi:x.1056/NEJMp1407639. PMID 25539104.
- ^ Neidich, Due east.; Neidich, A. B.; Axelrod, D. A.; Roberts, J. P. (2013). "Consumerist Responses to Scarcity of Organs for Transplant". Virtual Mentor. fifteen (11): 966–972. doi:10.1001/virtualmentor.2013.fifteen.eleven.pfor2-1311. PMID 24257089.
- ^ "Former Man United striker Andy Cole undergoes kidney transplant: Club ambassador has a condition called Focal Segmental Glomerulosclerosis". The Irish Times. 7 Apr 2017. Retrieved 7 April 2017.
- ^ "Andrew Cole: Former Manchester United and England star has kidney op". BBC News. seven April 2017. Retrieved vii April 2017.
- ^ Jepson, Anthony (iii September 2017). "Manchester United cracking Andy Cole thanks two old teammates equally he battles to regain full health". Manchester Evening News . Retrieved 6 November 2017.
- ^ "Coleman battled lifelong health woes: transplants, kidney bug - CNN.com". www.cnn.com . Retrieved 27 June 2019.
- ^ Dvorak, Petula (January 10, 2022). "He thought getting a new kidney in the pandemic would be impossible. His son's charabanc stepped up". The Washington Postal service. Washington, D.C. Archived from the original on 2022-01-xi.
External links [edit]
-
 Media related to Kidney transplantation at Wikimedia Commons
Media related to Kidney transplantation at Wikimedia Commons - Kidney transplantation at Curlie
- Kidney transplantation
Source: https://en.wikipedia.org/wiki/Kidney_donation
0 Response to "Requirements to Donate a Kidney to a Family Member"
Post a Comment